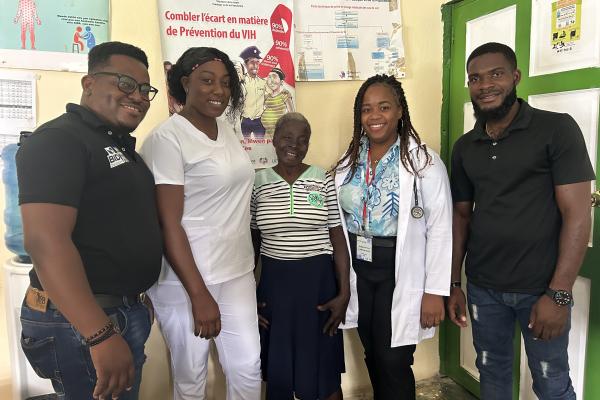
Wed Richy Pierre Noel is a pharmacist and HIV and tuberculosis program coordinator at Zanmi Lasante, Partners In Health’s sister organization in Haiti. He oversees the distribution of antiretrovirals in 13 hospitals and health centers in Plateau Central and Bas Artibonite. He works with the clinical teams to ensure that patients are screened, treated and accompanied until viral suppression is achieved. This work is made possible thanks to the ongoing support of partners such as PEPFAR.

Haiti has made major progress in the fight against HIV. At Zanmi Lasante sites, the majority of patients on treatment are now achieving viral suppression. The organization is making steady progress towards the global 95-95-95 targets. These advances are not theoretical. They translate into longer lives, parents able to care for their children and young people growing up with sustainable access to treatment.
This progress is measurable and independently recognized. On October 31, at the Ministry of Health’s HealthQual Forum in Artibonite, Zanmi Lasante was awarded first and third place among all quality improvement projects. The winning projects focused on the early renewal of ARVs to avoid treatment interruptions, and the active search for undiagnosed people. These results were achieved against a backdrop of insecurity, fuel shortages and limited road access. They show that when resources are available, they are used effectively.
The situation remains fragile. Haiti is going through one of the most serious security and economic crises in its history. Armed groups control essential roads. Health personnel often travel under threat. Deliveries of ARVs and laboratory supplies are regularly delayed. When this happens, teams find temporary solutions. But if funding is cut at the same time, the system cannot absorb both shocks. Stock-outs become more likely. Viral suppression rates fall. Resistance increases. Lives are lost.
A recent case clearly illustrates what’s at stake. A woman living with HIV had stopped attending her appointments. Community health workers went to her home and found her extremely weak, feverish, with a persistent cough. She had developed tuberculosis, which is very dangerous for people living with HIV. Her family couldn’t afford transport, so she stayed at home until she was close to death.

Zanmi Lasante staff took her to hospital, resumed her treatment, tested her for TB and immediately began therapy. She received nutritional and psychosocial support. Today, she is recovering. According to Richy, if the medication hadn’t been available or if the laboratory hadn’t been able to confirm tuberculosis, she wouldn’t have survived.
Here’s what U.S. funding makes possible every day in Haiti
- Continuous supply of ARVs in remote or unstable areas
- Laboratories able to measure viral load and detect tuberculosis or resistance early
- Community health workers who find patients, follow-up and prevent treatment failures
- Integrated HIV and TB care, nutritional support and psychological services
- Training of Haitian clinicians, pharmacists, nurses and community workers
When funding is interrupted, the effects are immediate. A simple delay in the supply of ARVs can lead to treatment interruption and the creation of resistance. Fewer community workers means more patients lost to follow-up. Without laboratories, it becomes impossible to monitor viral load or screen for tuberculosis. Years of progress can quickly disappear.
“We’re not asking for anything new. We’re asking to protect what’s been built. The system works, but only if it’s sustained.”
Despite insecurity, fuel shortages and political instability, Haiti’s healthcare workers continue their mission. They walk long distances to reach patients. They transport medicines on foot when vehicles can’t get through. They keep services open even when violence is close at hand. Their commitment is real, but it can’t replace drugs, lab tools or salaries.
Zanmi Lasante’s message to U.S. policymakers is clear. Investments in the fight against HIV in Haiti are yielding results. Viral suppression is possible. Quality of care is improving. Lives are being saved. Without continued PEPFAR support, these gains could be lost in a matter of months.
Continuing to fund these interventions is not an act of charity. It’s the difference between a functioning HIV care system and a humanitarian emergency.
The progress described here relies on constant resources, trained personnel and tools capable of rapidly identifying complications. To prevent the situation from turning upside down, every contribution counts. Supporting Zanmi Lasante means maintaining access to treatment, protecting the most vulnerable patients and preventing a brutal setback.